- Startseite
- Publikationen
- GIGA Focus
- Access to COVID-19 Vaccines and Medicines – a Global Public Good
GIGA Focus Global
Zugang zu COVID-19-Impfstoffen und Medikamenten: Ein globales öffentliches Gut
Nummer 4 | 2020 | ISSN: 1862-3581

New daily record numbers of infections worldwide exacerbate concerns about the impact of the COVID-19 pandemic on regions of the Global South. Weak health systems, vulnerable economies, and extreme inequalities threaten healthcare, livelihoods, and peace in many low- and middle-income countries. The risk of increasing infection rates remains imminent for all countries until a vaccine or medicine is available to everyone worldwide.
While many low-income countries urgently need to “flatten the curve”, rigid lockdown measures are difficult to impose in the vast informal sector and can mean a more imminent threat to lives and livelihoods by depriving millions of income and food.
COVID-19 has already led to a world economic crisis through the breakdown of trade and rapidly increasing debts, and will only aggravate global inequalities even further.
The key for slowing and eventually stopping the pandemic without lockdowns lies in the development of, and universal access to, effective drugs and vaccines, which are currently discussed on the highest political level as being “global public goods.”
An unprecedented initiative vis-à-vis the required collective action in global health is the Access to COVID-19 Tools Accelerator bringing together many important stakeholders in global health.
Whether stakeholders will meet their commitments on access is not clear yet, as a three-way conflict intensifies between those demanding access to health products as a global public good, pharmaceutical firms offering compromises but defending patent-based exclusive rights, and “vaccine nationalism” by individual states.
Policy Implications
This pandemic could be an opportunity to realise access to vaccines and medi-cines for all. The high-level public debate about medicines as a global public good is unprecedented, and there are promising examples of collective action. It remains to be seen whether national governments and pharmaceutical companies can be held accountable by the defenders of a global public good approach regarding their publicly voiced commitment to “access for all.”
Pathway and Impact of the Pandemic in the Global South
Recognising the pandemic nature of COVID-19 has led to great concerns about the problems of poor countries in dealing with the disease. Potentially catastrophic impacts are feared in particular in low- and a number of middle-income countries (LICs and MICs), with large groups of marginalised people in poor rural areas and urban slums. Other recent GIGA Foci have already highlighted the specific problems faced in Africa, Latin America, and the Middle East as a result of the pandemic (see “Related GIGA Publications”). It appears that food markets have been particular hubs of infection helping spread the virus in Latin American countries (Collyns et al. 2020). The countries of the Arabian Peninsula are now among those with the highest rates of infections per one million inhabitants. However, this might be skewed because of their comparatively high rate of testing. At the same time they exhibit a comparatively low death rate due to their highly developed health systems. While sub-Saharan Africa was less severely hit until early April compared to other parts of the world, the pandemic has since started to gain pace there. There is also an imminent risk that COVID-19 will lead to more violent conflict on the continent, as Basedau and Deitch (2020) outline.
By now, another hotspot of infection has developed in South Asia. India has 586,956 confirmed infections and 17,417 deaths (as of 1 July), with 8,826,585 tests conducted (meaning only about 0.64 per cent of the population have been tested so far). A rigidly imposed lockdown, wearing of face masks in major Indian cities and many states being compulsory, and internal travel restrictions have resulted in reported hardships linked to these measures. The lockdown led to an exodus of migrant workers desperately trying to reach their home villages. Kerala, on the other hand, is demonstrating that basic health system infrastructure and investments in human capital can make all the difference in controlling a pandemic even despite scarce resources: the state has a strong, highly decentralised public health system, clear risk communication, and effective community participation, all based on the enduring state welfare regime established by the Communist Party of India.
High rates of informal employment, weak health systems, and very limited testing capacities are only some of the reasons why this pandemic represents a critical challenge for many LICs and LMICs. For example, while Lombardy – a hard-hit region in Italy – had about 700 Intensive Care Unit beds for a population of 10.4 million people, Mali and Burkina Faso have less than 20 ventilators for respective populations almost twice as large (Haas and Teachout 2020). According to an Organisation for Economic Co-operation and Development (OECD) study (2020a), about 86 per cent of total employment in Africa is informal and 82 per cent of the population are without social protection. Another critical aspect concerns food supplies; though a report of the Food and Agricultural Organization states that recent harvests have been good and the outlook for staple crops is promising, it warns of “indirect effects such as disruption of livelihoods, food supply chains and access to food, basic services as well as humanitarian assistance” (2020: 6) – also affecting food supplies for the urban poor. The disruption of international trade affects the income of African exporters as well as the supply of essential imports.
The World Health Organization (WHO) regularly updates its guidance for countries on how to maintain essential health services in the face of the pandemic. Despite very different sociocultural and economic preconditions between the Global South and the Global North, the measures implemented in most high income countries (HICs) have been recommended as general coping mechanisms.
Collateral Damage of Focusing All Efforts on COVID-19
However, more and more politicians from LICs have articulated that they are not in a position to afford a strict lockdown. For one, an economic lockdown can be a more imminent threat to lives and livelihoods by depriving millions of income and food. As protesting traders in Ghana put it: “They knew the lockdown was needed to curb the spread of the virus but they were not in a position to survive it” (Akinwotu and Asiedu 2020).
Furthermore, a complete lockdown might not be warranted in many LICs for other reasons besides. Cash and Patel point out that “for the first time in the post-war history of epidemics, there is a reversal of which countries are most heavily affected by a disease pandemic” (2020: 1687). Many countries of the Global South exhibit a lower risk of COVID-19-related mortality since their populations are much younger. Since the beginning of the pandemic people in LICs and MICs have continued to die in the millions from numerous diseases that have been prevalent for much longer. For example, deaths among children under five from pneumonia in LICs and MICs were estimated at almost 900,000 for 2015 (McAllister et al. 2019). This number represents a reduction of 47 per cent during the Millennium Development Goal period since the year 2000, which is consistent with a decreasing prevalence of risk factors and increasing socio-economic development, prevention, and improved access to quality healthcare. The strong focus on fighting COVID-19 threatens to turn back the clock on years of progress and severely increase morbidity and mortality for many diseases. Vaccination campaigns, for example, have been suspended in many countries, and the cessation of public transport has specifically prevented poor people as well as healthcare workers from reaching medical facilities. For all these reasons, Cash and Patel (2020) emphasise that context is essential in controlling a pandemic and question the appropriateness of HIC strategies for peers with fewer resources.
Wealthier countries are now allegedly coming to the rescue of those less well-endowed – not least to mitigate effects resulting from their “one-size-fits-all” lockdown advice. At first sight, the international support announced by various institutions appears overwhelming. The G20 Action Plan (“Supporting the Global Economy Through the COVID-19 Pandemic”) presented on 15 April is the most comprehensive document of cooperation in the global fight against the pandemic. G20 members agreed on a suspension of debt service payments for the poorest countries during 2020. The International Monetary Fund (IMF) has developed a crisis response package offering a USD 1 trillion lending capacity and the World Bank and Regional Development Banks are offering emergency response packages of more than USD 200 billion. For African countries already suffering from increasing debt services in previous years this only means, however, a short-term easing of their foreign debt. In fact, by using the offered credits their foreign debt situation could become even more severe in the medium term.
Impact of Lockdowns on the Global Economy and Growing Inequalities
Since April, it has been frequently stated that the world economy will suffer its worst year since the Great Depression of the 1930s. Many of the lockdown measures are expected to have a long-term negative impact on national economies, as well as the global one, due to reduced trade and decreasing income in many sectors. The OECD (2020b) estimates a reduction of activity in the main economies of between 15 and 30 per cent of gross domestic product. Numerous countries will only be able to cope with the situation by incurring new foreign debts, which will not ease future development. The disruption of global value chains constitutes the potentially most significant impact on the structure of the world economy.
Public compensation payments for the impact of lockdown measures are intended to stabilise national economies, but they also adversely affect international competition. The payments – as seen particularly in European countries – have drawn criticism that they contribute to global inequalities, as stronger economies are in a better position to increase their competitiveness even further. Within the European Union, COVID-19 has had a particularly strong impact on the economic situation in Italy and Spain. This has resulted in a heated discussion on an EU response to the crisis and the pathway to realising acts of solidarity. At first, medical assistance within the EU came about very slowly. There has also been a long-running conflict over how to deal with the economic impact of the crisis – with some member countries opposing a “communitarisation of debts.”
If there are concerns about the aggravation of inequalities within the EU, this applies even more so to the economic divide between HICs on the one side and LICs and some highly affected LMICs on the other. While emergency credits are offered by international financial Institutions on favourable conditions, they imply the increasing indebtedness of the hardest-hit countries. In combination with other economic and social dimensions, this is bound to only further exacerbate growing global inequalities.
The social and economic impacts are already severe, and the worrying outlook for the second half of 2020 is somehow uniting people and governments across the globe. The need for collective action “not only” for humanitarian reasons seems obvious, and can present an opportunity for international collaboration never seen before. The key for slowing and eventually stopping the pandemic without economic lockdowns lies in the development of, and universal access to, effective drugs and vaccines. So far, international initiatives and developments give rise to cautious optimism.
Access to Health Products for COVID-19 – a Global Public Good
At the launch of the Access to COVID-19 Tools (ACT) Accelerator (WHO 2020a) in April, the currently largest alliance to finance medicines and vaccine research, United Nations Secretary-General António Guterres and German chancellor Angela Merkel called potential vaccines and medicines clear examples of “global public goods” (GPGs). When taking their statement and the concept of GPGs at face value, this would mean that a future vaccine would need to be both non-excludable – that is, universally available to everyone – and non-rival, as the immunisation of any person is beneficial to everybody else. Since public goods are not born of market dynamics, their provision depends on collective action. This raises the questions of the motivation for financing provisions, and the mechanisms of allocating globally available resources.
The insufficient support to fight other global humanitarian crises (e.g. to prevent major famines) makes collective action seem unlikely at first. At second glance, though, there might be a real opportunity at this point for pooling financial resources and efforts on a global level. Indeed world leaders have united to make an unprecedented commitment to working together in order to accelerate access to COVID-19-related health products and tests for all (WHO 2020b). Since the beginning of the pandemic there have been several international donor-pledging conferences raising billions of euros for vaccines and medicines on each occasion.
These commitments are a response to the severe impacts of the pandemic worldwide. The economic implications of fighting COVID-19 are not only devastating for many countries on a national level, but also expected to create severe turbulence within the global economy. The longer there are no other ways than a “lockdown” to effectively control the pandemic – other than adopting the cynical attitude of not caring too much about the deaths of primarily the old –, the more serious and prolonged the economic consequences will be, and the higher the risk of violent political conflicts.
Collective Action: Cooperation in Research and Development and Access to COVID-19 Health Products
Since March, global health governance impetuses have abounded in calls for cooperation in research and development (R&D) and universal access to medicines. Based on the “R&D Blueprint for Action to Prevent Epidemics” established in 2015, an international group of scientists was invited to Geneva in February 2020 “to assess the current level of knowledge about the new virus, agree on critical research questions that need to be answered urgently, and to find ways to work together to accelerate and fund priority research to curtail this outbreak and prepare for those in the future.” In February 2020, the Coalition for Epidemic Preparedness Innovation (CEPI, an initiative founded in Davos in 2017 by the governments of India and Norway), the Bill & Melinda Gates Foundation, the Wellcome Trust, the World Economic Forum, and the World Bank together launched a COVID-19 Vaccine Development Taskforce (see Table 1 below for a timeline of selected actions and statements by different stakeholders regarding access to COVID-19 tools).
On 18 March, the WHO started the “Solidarity” clinical trial for COVID-19 treatments with the participation of more than 100 member countries to compare four treatment options: remdesivir; lopinavir/ritonavir combined; lopinavir/ritonavir combined with interferon-beta; and, hydroxychloroquine (or chloroquine). Eventually, on 24 April, the WHO launched the above-mentioned ACT Accelerator, which integrates most actors in the field of vaccine development and finance – such as CEPI, Gavi, the Vaccine Alliance, the Global Fund, Unitaid, and the International Federation of Pharmaceutical Manufacturers & Associations (IFPMA). The ACT Accelerator mission statement implicitly includes self-criticism by some actors, in particular industry, regarding their positions in past conflicts, referring to the long process of securing access to HIV/AIDS medicines: “We remember lessons from the past, which have shown that even when effective tools are available to the world, too often some are protected, while others are not. This inequity is unacceptable – all tools to address COVID-19 must be available to all. In the fight against COVID-19, no one should be left behind” (WHO 2020a).
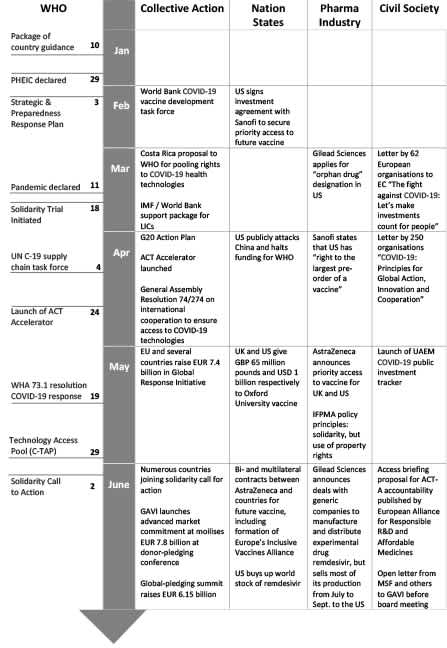
Collective Action Not Uncontested – Three-Way Conflict over Access to Medicines
Despite actors allegedly agreeing on the importance of equitable global access, there is a long-nursed conflict over access to medicines now clearly rearing its head amid abundant buzzwords like “GPGs,” “universal,” and “equitable.” We conceptualise this conflict as triangular (see Figure 1 below), with three major competing interests and stakeholder groups: (A) the pharmaceutical industry regarding patent-based exclusive rights; (B) certain nation states interested in securing health products first for themselves to speed up national recovery and (in some cases) to pursue hegemonic interests; and, (C) humanitarian, global, political, and economic interests to realise access to health products as GPGs. This latter interest is pursued by a diverse group of stakeholders, including patients, civil society organisations (CSOs), health workers, international organisations and foundations, and a number of LICs and MICs.
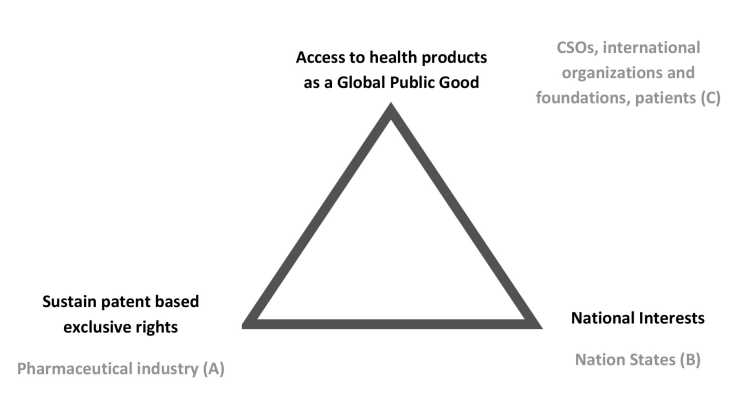
Although cooperation between multilateral institutions and transnational pharmaceutical corporations has been unusually broad with regards to the development of a COVID-19 vaccine, the distrust between CSOs and the pharmaceutical industry remains deep-seated. While the normative pressure to work together towards equitable access seems strong, CSOs fear that this putative common goal remains merely paying lip service in the absence of actual binding commitments. In fact, critical CSOs expect “a new wave of pro-IP [Intellectual Property] proposals from industry in the wake of COVID-19”; so far, a binding R&D convention is not in sight. CSOs have released several open letters demanding access for all, and accountability mechanisms for access commitments (see Table 1 above for examples). Universities allied for essential medicines (UAEM) found that most COVID-19 vaccine trials receive public funds and publishes a website that tracks whether COVID-19 research so funded is indeed accessible to all.
Conflicts around patent applications for remdesivir (Gilead Sciences) have already emerged, alongside Sanofi’s alleged commitment to produce vaccines prioritising the United States market. On 28 May, IFPMA published their “Policy Principles on COVID-19 Vaccines Initiative” – stressing the readiness of industry to support broad cooperation initiatives, but also insisting on supporting “expedite and effective product licensing approaches, recognizing that intellectual property has not been an impediment to pandemic response thus far” (2020).
But also national interests have already come into play, casting doubt on the sincerity of the loudly voiced calls for equitable access. In June, several countries and GAVI struck deals with AstraZeneca for the supply of a potential vaccine that is currently being tested by the University of Oxford. France, Germany, Italy, and the Netherlands joined up to what has been labelled Europe’s Inclusive Vaccines Alliance (IVA). The multilateral deal is supposed to provide “equitable access to all participating countries across Europe” (AstraZeneca 2020). This shift in phrasing – adding “participating,” and replacing “worldwide” with “across Europe” – could give the discourse a new direction and be an indication of weak accountability regarding commitment to worldwide access. The CEO of CEPI referred to these national deals as “vaccine nationalism,” describing the phenomenon as the biggest barrier to equitable access to COVID-19 vaccines (Saldinger 2020). By the end of June, the US government bought nearly all of Gilead Sciences’ production of remdesivir for July and 90 per cent of its August and September stocks too.
The language of the WHO’s WHA73 Resolution, sponsored by the EU and many other member countries, is equally telling. It uses strong wording on the right to health and calling for cooperation concerning intellectual property rights (IPRs) through existing mechanisms, for the voluntary pooling of patents and licensing of medicines and vaccines (WHO, COVID-19 Response, Document A73/CONF./1Rev.1). But it avoids any criticism on trade and IPR mechanisms, and falls short of suggesting concrete new solutions and binding commitments. Overall CSOs welcomed the draft, but stressed the need for more specific demands regarding transparency and the use of trade-related aspects of IPRs (TRIPS) flexibilities such as compulsory licensing – as exemplified in the Doha Declaration. Realising equitable access for all will depend on whether or not effective accountability mechanisms are established. In their absence, it will be impossible to hold organisations, corporations, and governments to account.
What might raise hope is the growing impact of shareholder value in the pharmaceutical industry; according to Reuters Business News, a group of institutional investors – holding more than EUR 1.9 trillion in assets – published a statement calling on 15 major pharmaceutical companies “to set aside rivalries and short-term interests and cooperate on finding solutions to the coronavirus.” Their statement further reads: “Enforcing patents, excessive price setting, not disclosing relevant findings or securing extended market exclusivity through, for example, orphan drug designation should not run counter to this responsibility” (Sterling 2020). This implies that the image of a company, stock prices, and its attractiveness for institutional investors might (at least in the short and medium run) be economically more rewarding than profits from selling patented products at high prices.
Will the GPG Be Delivered – and What After?
Looking at past processes of creating universal access to medicines and vaccines, such as the vaccination campaign to eradicate smallpox, this has always taken a long period of time to achieve – usually decades. Will the urgency of controlling COVID-19 provide the necessary conditions for a more rapid realisation of universal access (“no one left behind”)?
However the identified three-way conflict will play out, a core technical issue will make it difficult to achieve equal (meaning also, simultaneous) access to medicines and vaccines for people all over the world: the sheer impossibility of creating sufficient health products and providing the necessary medical infrastructure everywhere. The preconditions for a vaccination campaign include a cold chain for the storage and transport of dosages, as well as sterile needles and qualified health workers to administer them. Even though there have been many verbal commitments vis-à-vis collective action in the controlling of COVID-19, global inequalities will be hard to overcome. It remains to be seen whether stakeholders will live up to their commitments in realising vaccination against COVID-19 as a GPG and even reform access to medicines in a sustainable way – or if the observed vaccine nationalism and strong industry lobby will cement existing structures that uphold access to medicines as a privilege only for those who can afford it.
The severity and the all-encompassing nature of the COVID-19 crisis has led to the widespread conviction that it should be interpreted as an opportunity for a new start in global collective development. The point of departure here, however, is a paradox: on the one hand, it is seen as proof of the limits of globalisation, pointing to the impacts of the disruption of global value chains and an inward orientation among societies in fighting the disease; on the other, never before has there been a situation in which political discourses around the world have focused on almost the exact same political issues. Global discourses are dominated by the development of and access to COVID-19 vaccines and medicines, and by strategies to overcome the economic crisis – all heavily dependent on global cooperation.
Despite the urgent hope and indeed need for COVID-19 medicines and vaccines, Kohler and Mackey (2020) warn against bypassing existing regulatory safeguards in favour of earlier access to immature and possibly unsafe products. They also call for delegating responsibility to a supranational body that can establish a system to coordinate rational selection, procurement, access, and distribution across all countries. If the global community succeeds in overcoming national protectionism impulses and focuses rather on protecting people’s rights to equitable access instead of industry’s rights to patents, the current pandemic could be a game changer for access to medicines.
Fußnoten
References
Akinwotu, E., and Asiedu, K. (2020), Easing of Lockdown a Relief to Ghana’s Poor – Despite Fears it is Premature, in: The Guardian International Edition (2020), 3 May, www.theguardian.com/global-development/2020/may/03/coronavirus-easing-of-lockdown-a-relief-to-ghanas-poor-despite-fears-it-is-premature (20 May 2020).
AstraZeneca (2020), AstraZeneca to Supply Europe with up to 400 Million Doses of Oxford University’s Potential COVID-19 Vaccine, www.astrazeneca.com/media-centre/articles/2020/astrazeneca-to-supply-europe-with-up-to-400-million-doses-of-oxford-universitys-potential-covid-19-vaccine.html (19 June 2020).
Baker, B., (2020), Expect a Wave of Pro-IP Proposals from Industry in the Wake of the COVID-19. Health GAP, April 3, https://healthgap.org/expect-a-wave-of-pro-ip-proposals-from-industry-in-the-wake-of-the-covid-19/ (15 June 2020).
Cash, R., and Patel, V. (2020). Has COVID-19 Subverted Global Health?, in: The Lancet, 395 (10238), 1687-1688, www.thelancet.com/journals/lancet/article/PIIS0140-6736(20)31089-8/fulltext (15 June 2020).
Collyns, D., Daniels, J.P., Phillips, D. and Agren, D. (2020), "Hubs of Infection": How Covid-19 Spread through Latin America's Markets, in: The Guardian International Edition, 17 May, www.theguardian.com/world/2020/may/17/coronavirus-latin-america-markets-mexico-brazil-peru (15 June 2020).
Food an Agricultural Organization (2020), Addressing the Impacts of COVID-19 in Food Crises. Rome, April–December 2020, www.fao.org/documents/card/en/c/ca8497en/ (06 July).
Haas, A., and Teachout, M. (2020), Could the Economic Cost Outpace the Health Impact of COVID-19 in Africa?, International Growth Centre, 3 April, www.theigc.org/blog/could-the-economic-cost-outpace-the-health-impact-of-covid-19-in-africa/ (15 June).
IFPMA (2020), COVID-19 IFPMA Policy Principles on COVID-19 Vaccines Initiative, Geneva, www.ifpma.org/wp-content/uploads/2020/05/IFPMA_Policy_Principles_COVID-19_Vaccines_Initiative.pdf (06 July 2020).
Kohler, J. C., and Mackey, T. K. (2020), Why the COVID-19 Pandemic Should be a Call for Action to Advance Equitable Access to Medicines, in: BMC Medicine, 18, 1, 1-3, https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-020-01661-3 (06 July 2020).
McAllister, D. A., Liu, L., Shi, T., Chu, Y., Reed, C., Burrows, J., Adeloye, D., Rudan, I., Black, R. E., Campbell, H., & Nair, H. (2019), Global, Regional, and National Estimates of Pneumonia Morbidity and Mortality in Children Younger than 5 Years between 2000 and 2015: a Systematic Analysis, in: The Lancet. Global health, 7, 1, e47–e57, www.sciencedirect.com/science/article/pii/S2214109X1830408X?via%3Dihub (06 July 2020).
OECD (2020a), COVID-19 and Africa: Socio-economic Implications and Policy Responses (OECD Policy Responses to Coronavirus [COVID-19]), www.oecd.org/coronavirus/policy-responses/covid-19-and-africa-socio-economic-implications-and-policy-responses-96e1b282/ (06 July 2020).
OECD (2020b), Evaluating the Initial Impact of COVID-19 Containment Measures on Economic Activity (OECD Policy Responses to Coronavirus [COVID-19]), www.oecd.org/coronavirus/policy-responses/evaluating-the-initial-impact-of-covid-19-containment-measures-on-economic-activity-b1f6b68b/ (15 June 2020).
Saldinger, A. (2020), CEPI CEO: Scarcity, “Vaccine Nationalism” Biggest Barriers for COVID-19 Vaccine Access, 12 June, www.devex.com/news/cepi-ceo-scarcity-vaccine-nationalism-biggest-barriers-for-covid-19-vaccine-access-97466 (20 June 2020).
Sterling, T. (2020), Institutional Investors Tell Big Pharma to Cooperate on Coronavirus, Business News, www.reuters.com/article/us-health-coronavirus-investors-pharmace/institutional-investors-tell-big-pharma-to-cooperate-on-coronavirus-idUSKBN21Z1WZ (06 July 2020).
World Health Organization (2020a), Access to Covid-19 Tools (Act) Accelerator. Commitment and Call to Action, Geneva, www.who.int/publications/m/item/access-to-covid-19-tools-(act)-accelerator (06 July 2020).
World Health Organization (2020b), Global Leaders Unite to Ensure Everyone Everywhere Can Access New Vaccines, Tests and Treatments for COVID-19 (WHO Newsroom), Geneva, www.who.int/news-room/detail/24-04-2020-global-leaders-unite-to-ensure-everyone-everywhere-can-access-new-vaccines-tests-and-treatments-for-covid-19 (05 June 2020)
Gesamtredaktion GIGA Focus
Redaktion GIGA Focus Global
Lektorat GIGA Focus Global
Regionalinstitute
Forschungsschwerpunkte
Wie man diesen Artikel zitiert
Hein, Wolfgang, und Anne Paschke (2020), Zugang zu COVID-19-Impfstoffen und Medikamenten: Ein globales öffentliches Gut, GIGA Focus Global, 4, Hamburg: German Institute for Global and Area Studies (GIGA), https://nbn-resolving.org/urn:nbn:de:0168-ssoar-68332-2
Impressum
Der GIGA Focus ist eine Open-Access-Publikation. Sie kann kostenfrei im Internet gelesen und heruntergeladen werden unter www.giga-hamburg.de/de/publikationen/giga-focus und darf gemäß den Bedingungen der Creative-Commons-Lizenz Attribution-No Derivative Works 3.0 frei vervielfältigt, verbreitet und öffentlich zugänglich gemacht werden. Dies umfasst insbesondere: korrekte Angabe der Erstveröffentlichung als GIGA Focus, keine Bearbeitung oder Kürzung.
Das German Institute for Global and Area Studies (GIGA) – Leibniz-Institut für Globale und Regionale Studien in Hamburg gibt Focus-Reihen zu Afrika, Asien, Lateinamerika, Nahost und zu globalen Fragen heraus. Der GIGA Focus wird vom GIGA redaktionell gestaltet. Die vertretenen Auffassungen stellen die der Autorinnen und Autoren und nicht unbedingt die des Instituts dar. Die Verfassenden sind für den Inhalt ihrer Beiträge verantwortlich. Irrtümer und Auslassungen bleiben vorbehalten. Das GIGA und die Autorinnen und Autoren haften nicht für Richtigkeit und Vollständigkeit oder für Konsequenzen, die sich aus der Nutzung der bereitgestellten Informationen ergeben.